Get the free note client change
Show details
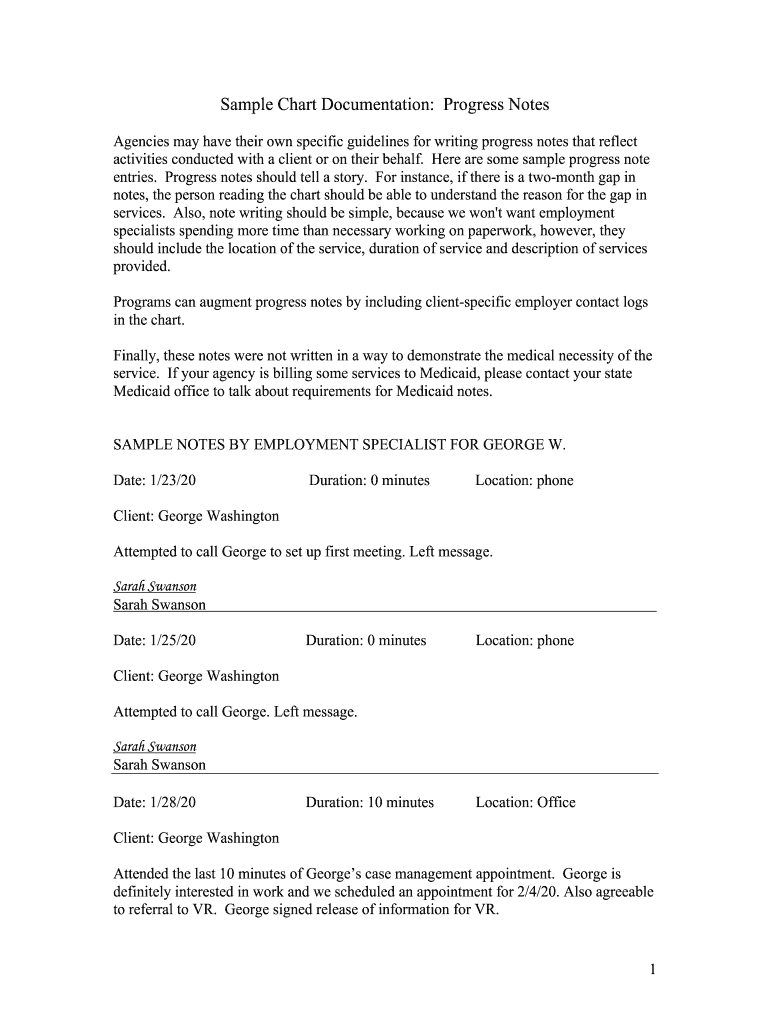
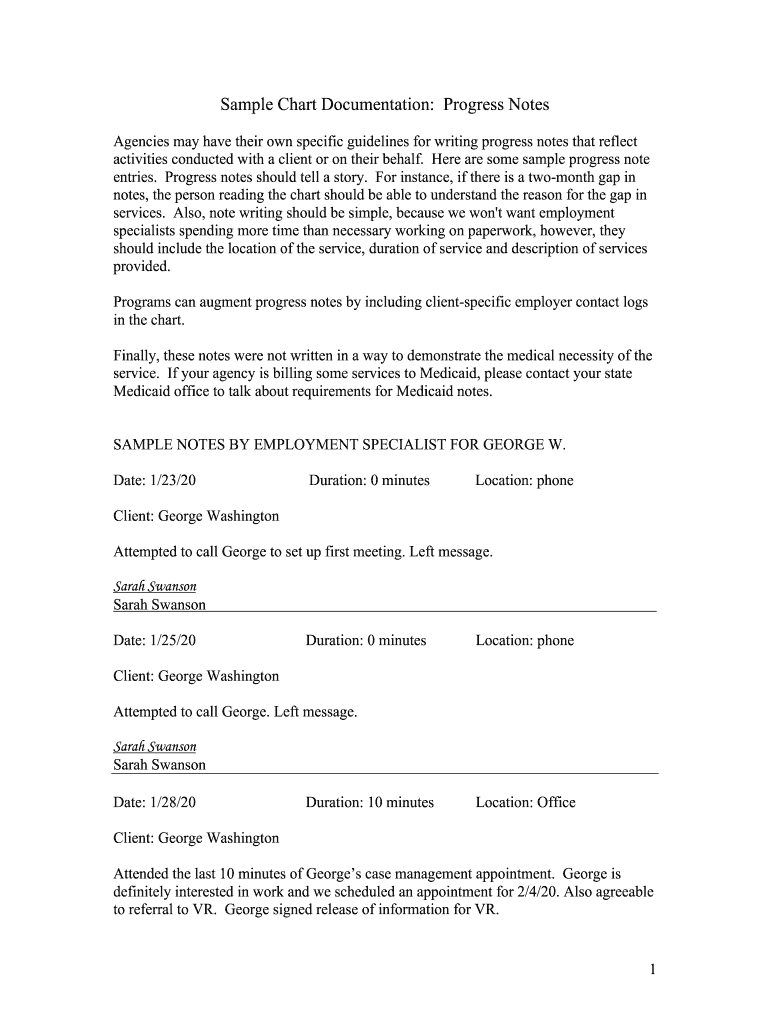
Progress notes should tell a story. For instance if there is a two-month gap in notes the person reading the chart should be able to understand the reason for the gap in services. Sample Chart Documentation Progress Notes Agencies may have their own specific guidelines for writing progress notes that reflect activities conducted with a client or on their behalf. Here are some sample progress note entries. Also note writing should be simple because we won t want employment specialists spending...
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign note chart pages form
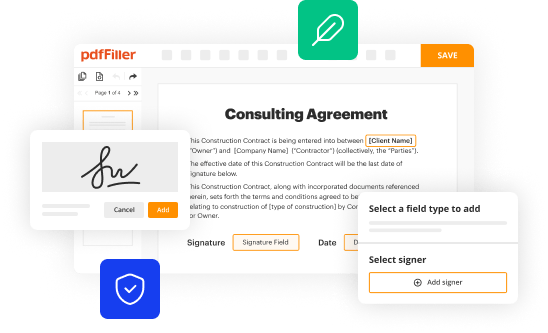
Edit your human sample notes form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your reflected chart form via URL. You can also download, print, or export forms to your preferred cloud storage service.
Editing human progress documentation online
Here are the steps you need to follow to get started with our professional PDF editor:
1
Log in to your account. Click on Start Free Trial and register a profile if you don't have one.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
Edit sample documentation notes pdf form. Add and replace text, insert new objects, rearrange pages, add watermarks and page numbers, and more. Click Done when you are finished editing and go to the Documents tab to merge, split, lock or unlock the file.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
pdfFiller makes working with documents easier than you could ever imagine. Create an account to find out for yourself how it works!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out sample chart progress notes blank form
How to fill out Sample Chart Documentation Progress Notes
01
Begin by entering the patient's name and date of the session at the top of the document.
02
Indicate the type of session (e.g., initial evaluation, follow-up visit).
03
Fill out the reason for the visit, summarizing key issues or concerns.
04
Document the patient's progress since the last visit, noting any changes in symptoms or behavior.
05
Include any interventions used during the session and the patient's response to them.
06
Set goals for future sessions and outline a treatment plan if applicable.
07
Sign and date the document at the bottom.
Who needs Sample Chart Documentation Progress Notes?
01
Healthcare providers documenting patient care.
02
Administrative staff managing patient records.
03
Insurance companies for claims processing.
04
Legal professionals for compliance and legal matters.
Fill
human progress notes template
: Try Risk Free
People Also Ask about chart documentation progress
What is the most recommended format for documenting progress notes?
The SOAP (Subjective, Objective, Assessment, and Plan) note is probably the most popular format of progress note and is used in almost all medical settings.
How do you write progress notes?
Progress notes record the date, location, duration, and services provided, and include a brief narrative. Documentation should substantiate the duration and frequency of service delivery. The narrative should describe the following elements: Client's symptoms/behaviors.
What are the formats for progress notes?
There are several widely used formats for progress notes that can provide a template for making your note-keeping more efficient, while including all of the necessary key points: DAP (Description, Assessment, Plan) BIRP (Behavior, Intervention, Response, Plan) SOAP (Subjective, Objective, Assessment, Plan)
What is the best way to write progress notes?
Progress notes record the date, location, duration, and services provided, and include a brief narrative. Documentation should substantiate the duration and frequency of service delivery. The narrative should describe the following elements: Client's symptoms/behaviors.
What is a simple progress note?
Progress notes cover three basic categories of information: what you observe about the client in session, what it means, and what you (or your client) are going to do about it. They can also be completed collaboratively with the client, to help establish a therapeutic alliance.
How do you do progress notes in Word?
Progress Notes are brief narrative entries written to record negative and positive events relating to residents.Be Objective and Brief Objective phrases are those based on observation and presented as facts. They should not be written based on prejudices or influenced by emotional outpour.
Our user reviews speak for themselves
Read more or give pdfFiller a try to experience the benefits for yourself
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send chart progress notes pdf to be eSigned by others?
Once your note pages information is complete, you can securely share it with recipients and gather eSignatures with pdfFiller in just a few clicks. You may transmit a PDF by email, text message, fax, USPS mail, or online notarization directly from your account. Make an account right now and give it a go.
How do I fill out the chart pages form on my smartphone?
On your mobile device, use the pdfFiller mobile app to complete and sign sample chart progress notes. Visit our website (https://edit-pdf-ios-android.pdffiller.com/) to discover more about our mobile applications, the features you'll have access to, and how to get started.
Can I edit note client on an Android device?
With the pdfFiller mobile app for Android, you may make modifications to PDF files such as progress notes template. Documents may be edited, signed, and sent directly from your mobile device. Install the app and you'll be able to manage your documents from anywhere.
What is Sample Chart Documentation Progress Notes?
Sample Chart Documentation Progress Notes are structured records that detail the ongoing progress and treatment of a patient throughout their healthcare journey.
Who is required to file Sample Chart Documentation Progress Notes?
Healthcare providers, including doctors, nurses, and therapists involved in patient care, are required to file Sample Chart Documentation Progress Notes.
How to fill out Sample Chart Documentation Progress Notes?
To fill out Sample Chart Documentation Progress Notes, healthcare providers should include pertinent patient information, details of the patient's condition, treatment provided, and any follow-up plans or recommendations.
What is the purpose of Sample Chart Documentation Progress Notes?
The purpose of Sample Chart Documentation Progress Notes is to ensure accurate tracking of a patient's progress, facilitate communication among healthcare providers, and support continuity of care.
What information must be reported on Sample Chart Documentation Progress Notes?
Information that must be reported includes patient demographics, date of the visit, observations, treatment interventions, patient response to treatment, and any future appointments or referrals.
Fill out your Sample Chart Documentation Progress Notes online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
Human Progress Notes is not the form you're looking for?Search for another form here.
Keywords relevant to sample chart documentation
Related to sample chart progress
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.